Relative risk
The relative risk (RR) or risk ratio is the ratio of the probability of an outcome in an exposed group to the probability of an outcome in an unexposed group. Together with risk difference and odds ratio, relative risk measures the association between the exposure and the outcome.[1]
Statistical use and meaning
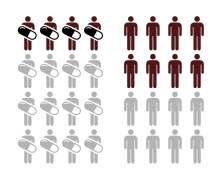
Relative risk is used in the statistical analysis of the data of ecological, cohort, medical and intervention studies, to estimate the strength of the association between exposures (treatments or risk factors) and outcomes.[2] Mathematically, it is the incidence rate of the outcome in the exposed group, , divided by the rate of the unexposed group, .[3] As such, it is used to compare the risk of an adverse outcome when receiving a medical treatment versus no treatment (or placebo), or for environmental risk factors. For example, in a study examining the effect of the drug apixaban on the occurrence of thromboembolism, 8.8% of placebo-treated patients experienced the disease, but only 1.7% of patients treated with the drug did, so the relative risk is .19 (1.7/8.8): patients receiving apixaban had 19% the disease risk of patients receiving the placebo.[4] In this case, apixaban is a protective factor rather than a risk factor, because it reduces the risk of disease.
Assuming the causal effect between the exposure and the outcome, values of relative risk can be interpreted as follows:[2]
- RR = 1 means that exposure does not affect the outcome
- RR < 1 means that the risk of the outcome is decreased by the exposure, which is a "protective factor"
- RR > 1 means that the risk of the outcome is increased by the exposure, which is a "risk factor"
As always, correlation does not mean causation and care must be taken to avoid reverse causality. The relative risk of having cancer when in the hospital versus at home, for example, would be greater than 1, but that is because havnig cancer causes people to go to the hospital.
Usage in reporting
Relative risk is commonly used to present the results of randomized controlled trials.[5] This can be problematic, if the relative risk is presented without the absolute measures, such as absolute risk, or risk difference.[6] In cases where the base rate of the outcome is low, large or small values of relative risk may not translate to significant effects, and the importance of the effects to the public health can be overestimated. Equivalently, in cases where the base rate of the outcome is high, values of the relative risk close to 1 may still result in a significant effect, and their effects can be underestimated. Thus, presentation of both absolute and relative measures is recommended.[7]
Inference
Relative risk can be estimated from a 2×2 contingency table:
| Group | ||
|---|---|---|
| Intervention (I) | Control (C) | |
| Events (E) | IE | CE |
| Non-events (N) | IN | CN |
The point estimate of the relative risk is
The sampling distribution of the is closer to normal than the distribution of RR,[8] with standard error
The confidence interval for the is then
where is the standard score for the chosen level of significance[9][10]. To find the confidence interval around the RR itself, the two bounds of the above confidence interval can be exponentiated.[9]
In regression models, the exposure is typically included as an indicator variable along with other factors that may affect risk. The relative risk is usually reported as calculated for the mean of the sample values of the explanatory variables.
Comparison to the odds ratio

The relative risk is different from the odds ratio, although the odds ratio asymptotically approaches the relative risk for small probabilities of outcomes. If IE is substantially smaller than IN, then IE/(IE + IN) IE/IN. Similarly, if CE is much smaller than CN, then CE/(CN + CE) CE/CN. Thus, under the rare disease assumption
In practice the odds ratio is commonly used for case-control studies, as the relative risk cannot be estimated.[1]
In fact, the odds ratio has much more common use in statistics, since logistic regression, often associated with clinical trials, works with the log of the odds ratio, not relative risk. Because the (natural log of the) odds of a record is estimated as a linear function of the explanatory variables, the estimated odds ratio for 70-year-olds and 60-year-olds associated with the type of treatment would be the same in logistic regression models where the outcome is associated with drug and age, although the relative risk might be significantly different.
Since relative risk is a more intuitive measure of effectiveness, the distinction is important especially in cases of medium to high probabilities. If action A carries a risk of 99.9% and action B a risk of 99.0% then the relative risk is just over 1, while the odds associated with action A are more than 10 times higher than the odds with B.
In statistical modelling, approaches like Poisson regression (for counts of events per unit exposure) have relative risk interpretations: the estimated effect of an explanatory variable is multiplicative on the rate and thus leads to a relative risk. Logistic regression (for binary outcomes, or counts of successes out of a number of trials) must be interpreted in odds-ratio terms: the effect of an explanatory variable is multiplicative on the odds and thus leads to an odds ratio.
Bayesian interpretation
We could assume a disease noted by , and no disease noted by , exposure noted by , and no exposure noted by . The relative risk can be written as
This way the relative risk can be interpreted in Bayesian terms as the posterior ratio of the exposure (i.e. after seeing the disease) normalized by the prior ratio of exposure.[11] If the posterior ratio of exposure is similar to that of the prior, the effect is approximately 1, indicating no association with the disease, since it didn't change beliefs of the exposure. If on the other hand, the posterior ratio of exposure is smaller or higher than that of the prior ratio, then the disease has changed the view of the exposure danger, and the magnitude of this change is the relative risk.
Numerical example
| Quantity | Experimental group (E) | Control group (C) | Total |
|---|---|---|---|
| Events (E) | EE = 15 | CE = 100 | 115 |
| Non-events (N) | EN = 135 | CN = 150 | 285 |
| Total subjects (S) | ES = EE + EN = 150 | CS = CE + CN = 250 | 400 |
| Event rate (ER) | EER = EE / ES = 0.1, or 10% | CER = CE / CS = 0.4, or 40% | — |
| Variable | Abbr. | Formula | Value |
|---|---|---|---|
| Absolute risk reduction | ARR | CER − EER | 0.3, or 30% |
| Number needed to treat | NNT | 1 / (CER − EER) | 3.33 |
| Relative risk (risk ratio) | RR | EER / CER | 0.25 |
| Relative risk reduction | RRR | (CER − EER) / CER, or 1 − RR | 0.75, or 75% |
| Preventable fraction among the unexposed | PFu | (CER − EER) / CER | 0.75 |
| Odds ratio | OR | (EE / EN) / (CE / CN) | 0.167 |
See also
References
- ^ a b Sistrom CL, Garvan CW (January 2004). "Proportions, odds, and risk". Radiology. 230 (1): 12–9. doi:10.1148/radiol.2301031028. PMID 14695382.
- ^ a b Carneiro, Ilona. (2011). Introduction to epidemiology. Howard, Natasha. (2nd ed.). Maidenhead, Berkshire: Open University Press. p. 27. ISBN 978-0-335-24462-1. OCLC 773348873.
- ^ Bruce, Nigel, 1955- (29 November 2017). Quantitative methods for health research : a practical interactive guide to epidemiology and statistics. Pope, Daniel, 1969-, Stanistreet, Debbi, 1963- (Second ed.). Hoboken, NJ. p. 199. ISBN 978-1-118-66526-8. OCLC 992438133.
{{cite book}}: CS1 maint: location missing publisher (link) CS1 maint: multiple names: authors list (link) CS1 maint: numeric names: authors list (link) - ^ Motulsky, Harvey (2018). Intuitive biostatistics : a nonmathematical guide to statistical thinking (Fourth ed.). New York. p. 266. ISBN 978-0-19-064356-0. OCLC 1006531983.
{{cite book}}: CS1 maint: location missing publisher (link) - ^ Nakayama T, Zaman MM, Tanaka H (April 1998). "Reporting of attributable and relative risks, 1966-97". Lancet. 351 (9110): 1179. doi:10.1016/s0140-6736(05)79123-6. PMID 9643696. S2CID 28195147.
- ^ Noordzij M, van Diepen M, Caskey FC, Jager KJ (April 2017). "Relative risk versus absolute risk: one cannot be interpreted without the other". Nephrology, Dialysis, Transplantation. 32 (suppl_2): ii13–ii18. doi:10.1093/ndt/gfw465. PMID 28339913.
- ^ Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG (March 2010). "CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials". BMJ. 340: c869. doi:10.1136/bmj.c869. PMC 2844943. PMID 20332511.
- ^ "Standard errors, confidence intervals, and significance tests". StataCorp LLC.
- ^ a b Szklo, Moyses; Nieto, F. Javier (2019). Epidemiology : beyond the basics (4th. ed.). Burlington, Massachusetts: Jones & Bartlett Learning. p. 488. ISBN 9781284116595. OCLC 1019839414.
- ^ Katz, D.; Baptista, J.; Azen, S. P.; Pike, M. C. (1978). "Obtaining Confidence Intervals for the relative risk in Cohort Studies". Biometrics. 34 (3): 469–474. doi:10.2307/2530610. JSTOR 2530610.
- ^ Armitage P, Berry G, Matthews JN (2002). Armitage P, Berry G, Matthews J (eds.). Statistical Methods in Medical Research. Vol. 64 (Fourth ed.). Blackwell Science Ltd. p. 1168. doi:10.1002/9780470773666. ISBN 978-0-470-77366-6. PMC 1812060.
{{cite book}}:|journal=ignored (help)